
Ireland Biocompatibility Testing
We know you are looking for a local biocompatibility testing laboratory in Ireland, but we would like to recommend our JJR Laboratory. Compared to local testing labs in Ireland, we can help you save 50% on certification testing costs. Additionally, we are a fully accredited institution recognized by both the FDA and CE.
Biocompatibility testing is a crucial step in ensuring the safety of medical devices when they come into contact with the human body. Whether it’s surgical instruments, implants, or in vitro diagnostic devices, neglecting this step can lead to delays in registration or, in the worst case, product recalls or legal disputes.
As a professional team in medical device consulting, we understand the pain points of companies during the testing phase—how to complete tests efficiently, how to select compliant solutions, and how to avoid potential pitfalls.
This article will provide a comprehensive overview of biocompatibility testing from three main perspectives: regulations, processes, and common issues. Our goal is to help you understand biocompatibility testing and accelerate your product's compliance and market launch!
Biocompatibility Testing: The "Safety Passport" for Medical Devices
1.1 What is Biocompatibility Testing?
Biocompatibility testing (Biocompatibility Testing) refers to a series of experiments to assess whether medical devices cause toxicity, irritation, sensitization, or other adverse reactions when in contact with human tissue, blood, or body fluids. The core objective is to validate the safety of materials and ensure the safety of patients and healthcare providers.
1.2 Why is it Necessary? — Regulatory Requirements
International:
- European Union (MDR): Testing according to ISO 10993 series standards.
- United States (FDA): Follows ISO 10993 and FDA guidelines.
- Other regions: Japan (JPAL), South Korea (MFDS), and other countries also consider biocompatibility a necessary requirement for registration.
1.3 Which Products Require Testing?
- Direct Contact: Catheters, implants, surgical instruments, dressings, etc.
- Indirect Contact: In vitro diagnostic reagent containers, dialysis device tubing, etc.
- High-Risk Scenarios: Long-term implants (e.g., heart stents), blood-contacting devices (e.g., heart-lung machines) require more stringent testing.
Overview of the Biocompatibility Testing Process
Material Classification and Contact Type Assessment
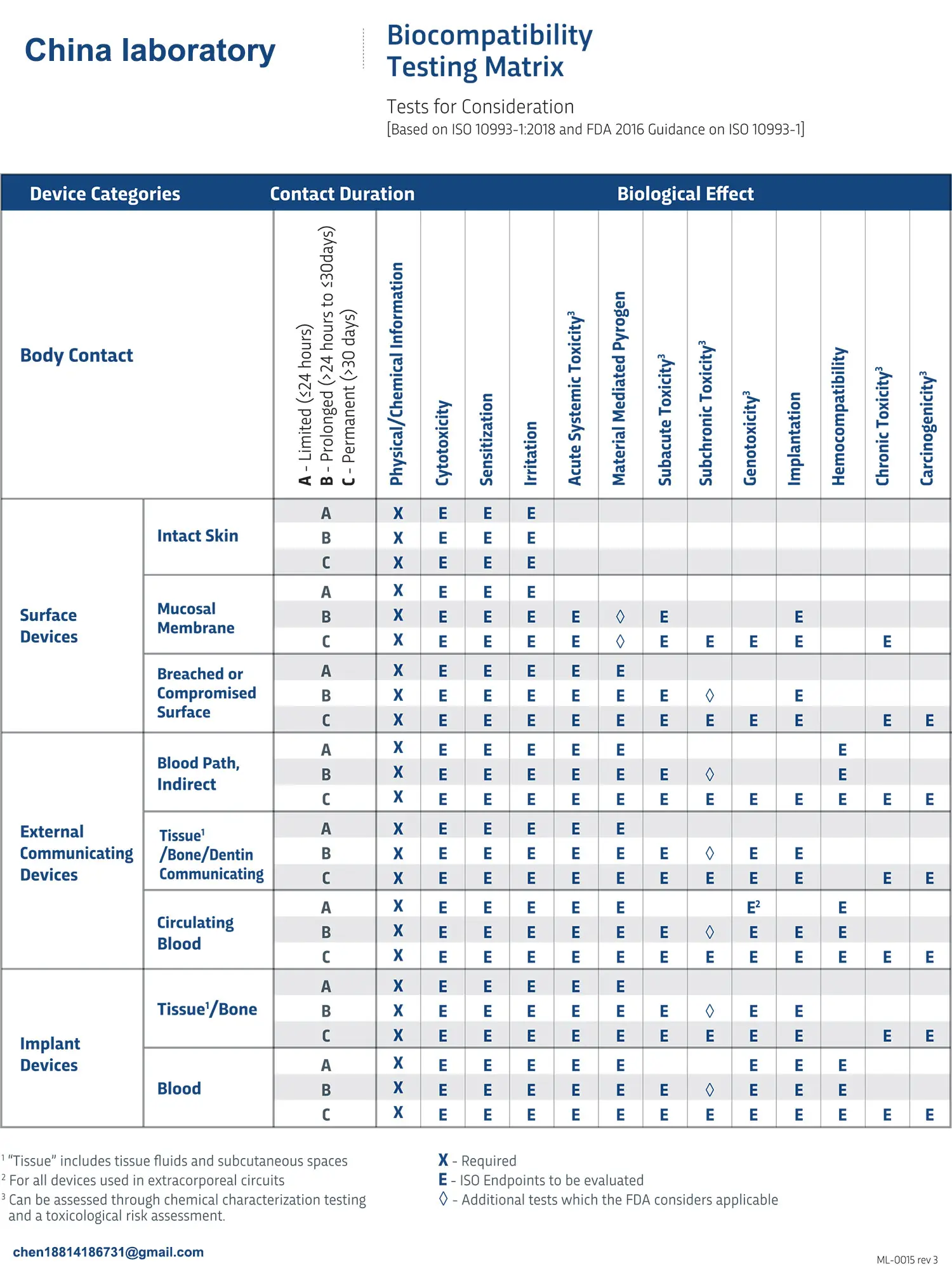
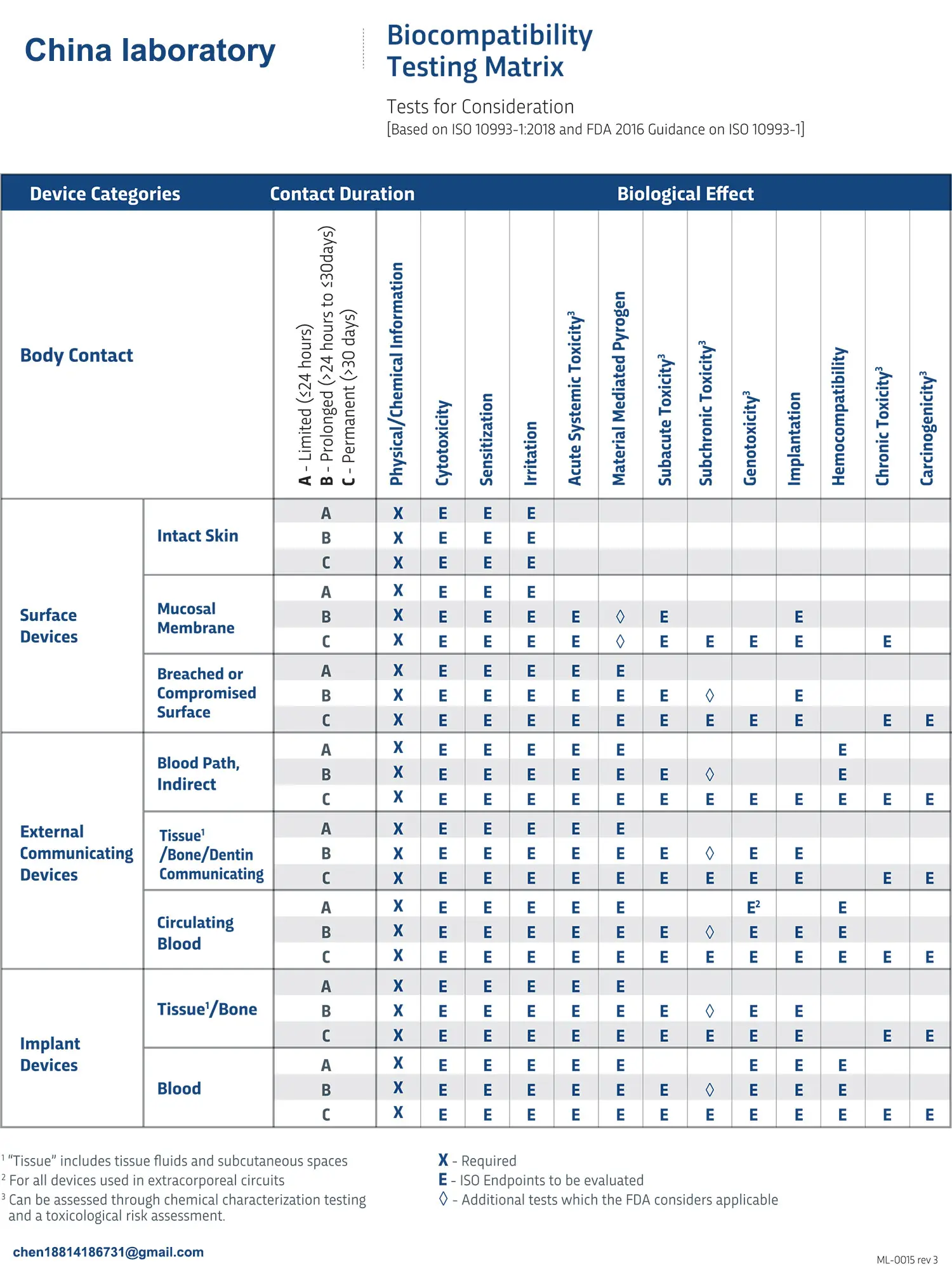
According to ISO 10993-1:2018, it’s essential to identify the nature (surface contact, implantation), duration (short-term, long-term), and material composition of the device to determine the necessary tests.
Example: A disposable syringe (short-term contact) only requires cytotoxicity and sensitization testing, while a joint prosthesis (long-term implant) requires additional evaluations for genotoxicity, chronic toxicity, etc.
Test Project Selection
The ISO 10993 series standards outline over 10 types of tests, commonly including:
- Cytotoxicity: Evaluate material's cytotoxic effects
- Skin Sensitization: Check for allergic reactions
- Irritation/Intradermal Reaction: Test for skin or tissue irritation
- Hemocompatibility: Analyze effects on blood components
- Genotoxicity: Check for genetic mutations
- Subchronic/Chronic Toxicity: Assess long-term toxicity effects
Laboratory Testing and Report
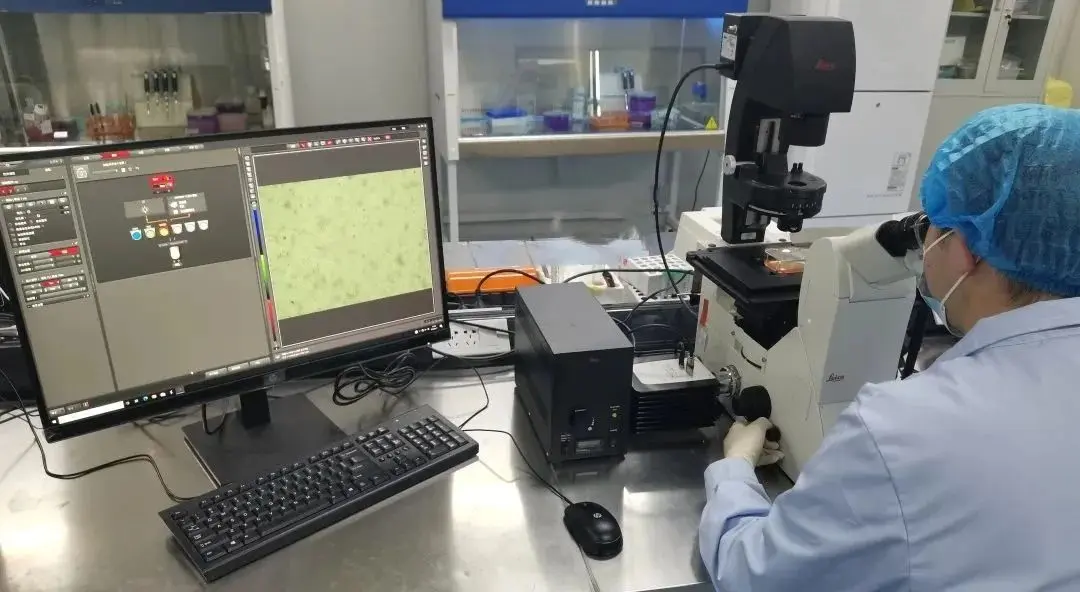
- Choosing a compliant laboratory: The lab must be accredited by CNAS, CMA, or have GLP certification (required for international registration).
- Testing duration and costs: Basic tests take about 4-8 weeks, with costs ranging from $2,300 to $6,000; complex projects (e.g., long-term implants) may take several months and cost over $15,000.
Report Review and Submission
The test report must be integrated into the medical device’s technical documentation and undergo rigorous review by regulatory agencies or notified bodies.
Common Misconceptions and Pitfall Avoidance Tips
Misconception 1: "The raw material supplier has already provided a test report, so no need for retesting."
- Truth: Raw material reports do not equal finished product reports! Manufacturing processes (e.g., sterilization, coating) can alter the material’s properties, and the final product must be tested.
Misconception 2: "The more tests, the better."
- Truth: Over-testing wastes time and money! Tests should be scientifically selected based on contact type and risk level.
Pitfall Avoidance Strategy:
- Early involvement: Collaborate with biocompatibility experts during the R&D phase to optimize material selection.
- Data exemptions: Use literature reviews or equivalence arguments to reduce redundant testing (e.g., when materials are identical to already approved products).
- Risk management: Integrate test results into a risk management system following ISO 14971.
Biocompatibility testing is the cornerstone of medical device safety and a necessary step for companies to comply with regulations. By choosing a professional partner, companies can significantly reduce risks and accelerate their product’s time to market.
Email:hello@jjrlab.com
Write your message here and send it to us
 Toothbrush FDA Certification Testing
Toothbrush FDA Certification Testing
 Snoring Device FDA 510k Standard Testing
Snoring Device FDA 510k Standard Testing
 Single Use Intravenous Catheter Certification Test
Single Use Intravenous Catheter Certification Test
 Silicone Material Product Compliance Certification
Silicone Material Product Compliance Certification
 What to Do If Cytotoxicity Test Results Are Positi
What to Do If Cytotoxicity Test Results Are Positi
 ISO 10993:5 Cytotoxicity Testing Methods
ISO 10993:5 Cytotoxicity Testing Methods
 FDA ISO 10993-1 Biocompatibility Evaluation Guidel
FDA ISO 10993-1 Biocompatibility Evaluation Guidel
 In Vitro Cytotoxicity Testing for Medical Devices
In Vitro Cytotoxicity Testing for Medical Devices
Leave us a message
24-hour online customer service at any time to respond, so that you worry!




