
How to Choose Biocompatibility Testing Items?
What is Biocompatibility?
Biocompatibility of medical devices refers to the ability of a device to interact with the host in a specific environment and location, either directly or indirectly, without causing harmful effects. It can also be understood as the biological performance of a device in a living organism, which remains stable and is not rejected or destroyed by the host’s various systems during static or dynamic changes. "Biocompatibility" and "biological incompatibility" are not inherent or absolute "labels" of materials; biocompatibility is a dynamic concept that must be evaluated based on the material’s specific properties and the particular clinical application scenario.
Classification Based on Medical Device Usage
Surface Contact Medical Devices
Surface contact medical devices can be further classified based on the nature of their contact. The three main categories are:
- Contact with Intact Skin: Common products include compression bandages, fixation bands, medical gloves, etc.
- Contact with Intact Mucosa: Common products include contact lenses, catheters, endotracheal tubes, bronchoscopes, and certain dentures.
- Contact with Wounds or Other Damaged Body Surfaces: Common products include band-aids, dressings for ulcers, or sealing patches.
External Access Medical Devices
External access medical devices can be classified into three categories:
- Devices not in direct contact with blood, but used to introduce fluids into the vascular system: Examples include infusion devices, extensions, transfer devices, and blood transfusion equipment.
- Devices that contact tissues, bones, or dental pulp/dentin: Examples include laparoscopes, arthroscopes, drainage systems, dental filling materials, and skin staples.
- Devices that come into direct contact with circulating blood: Common products include intravascular catheters, temporary pacing electrodes, oxygenators, extracorporeal oxygenator tubing, and dialysis devices.
Implantable Medical Devices
Implantable devices can be classified based on their application location:
- Devices that primarily contact bone or tissues and tissue fluids: Common products include orthopedic screws, plates, and artificial joints; devices that come into contact with tissues and tissue fluids include pacemakers, implantable drug delivery devices, artificial tendons, and breast implants.
- Devices that primarily contact circulating blood within the cardiovascular system: Common products include pacemaker electrodes, artificial arteriovenous fistulas, heart valves, artificial blood vessels, and ventricular assist devices.
Classification by Duration of Contact
Medical devices can be classified based on their contact duration as follows:
- Short-term contact (A): Devices that come into contact once, multiple times, or repeatedly with a cumulative duration of less than 24 hours.
- Long-term contact (B): Devices that come into contact once, multiple times, or repeatedly with a cumulative duration of more than 24 hours but less than 30 days.
- Persistent contact (C): Devices that come into contact once, multiple times, or repeatedly with a cumulative duration of more than 30 days.
- Instantaneous contact devices: These devices have very brief contact with the human body (e.g., surgical scalpels or hypodermic needles used for less than 1 minute), and typically do not require biocompatibility testing. However, some materials, such as coatings or lubricants, may remain in contact with the body after the device is removed, requiring further biocompatibility evaluation.
- Devices with multiple contact durations: If a material or device falls under more than one duration category, more stringent testing and evaluation are required. For devices that are expected to undergo multiple uses, the classification should consider the cumulative effect and the total time of contact. Additionally, if a device is expected to undergo changes during its lifespan, such as polymerization or degradation in situ, each of the different states of the device should be evaluated (e.g., initial components, intermediate reaction products, fully polymerized materials, and degradation products).
How to Choose Biocompatibility Testing Items
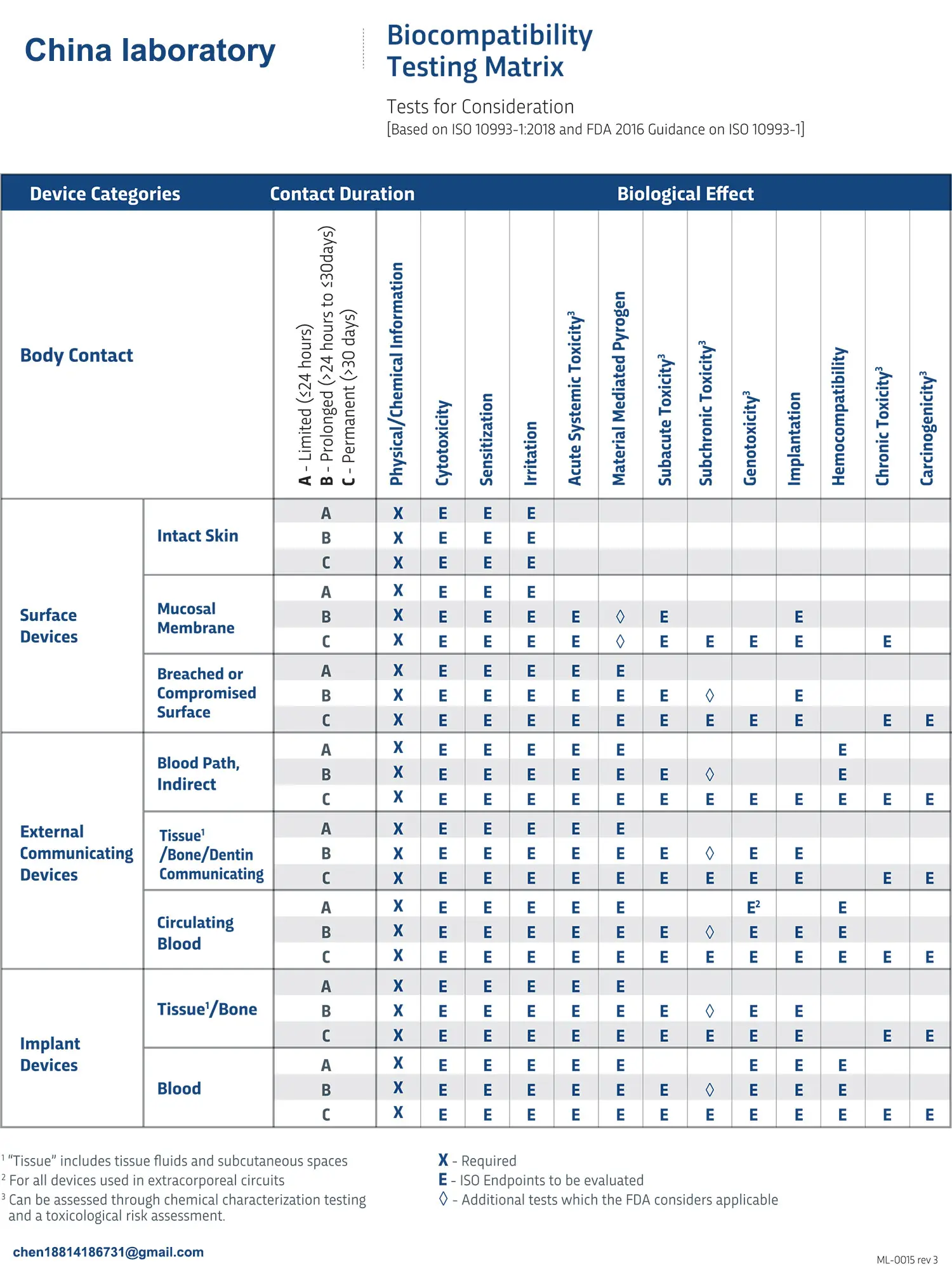
Once the medical device classification is determined according to the above contact properties and durations, refer to Annex A, Table 1 of ISO 10993 to find the corresponding biocompatibility testing items for the device.
Choosing a Testing Institution
When selecting a biocompatibility testing institution, medical device companies should consider not only the testing cycle and costs but also the qualifications of the testing institution. For products that are fully compliant with national or industry standards, the testing institution should possess the relevant national CMA qualifications. For products where testing requirements partially involve national or industry standards, the testing institution must have the necessary testing capabilities for the relevant tests and include a self-declaration in the testing report.
About Us
China JJR Laboratory operates toxicology, microbiology, and molecular biology laboratories. It is primarily responsible for testing, research, registration, and development of medical devices, disinfectants, cosmetics, chemicals, food/health foods, food contact materials, production water, disposable sanitary products, fire safety products, and more. JJR is a national testing institution for cosmetic and health food filing and inspection. Routine testing services include microbiological testing, bactericidal activity, skin irritation, eye irritation, phototoxicity, skin sensitization, pyrogen testing, cytotoxicity, genotoxicity, acute toxicity, sub-acute/sub-chronic toxicity, skin/muscle implantation, reproductive/developmental toxicity, chronic toxicity/carcinogenicity, toxicokinetics, and functional evaluation. JJR has over 500 CNAS/CMA accreditation capabilities and over 1,000 relevant testing standards.
Email:hello@jjrlab.com
Write your message here and send it to us
 When Can FCC ID Modifications Be Filed?
When Can FCC ID Modifications Be Filed?
 LoRa Certification Testing Laboratory
LoRa Certification Testing Laboratory
 Blood Pressure Monitor Certification Testing Servi
Blood Pressure Monitor Certification Testing Servi
 ECG Device Certification Testing
ECG Device Certification Testing
 Pulse Oximeter Certification and Testing Standards
Pulse Oximeter Certification and Testing Standards
 IVD Medical Device GB 4793:2024 Test Report
IVD Medical Device GB 4793:2024 Test Report
 IECEE CBTL Testing Laboratory for IVD Medical Devi
IECEE CBTL Testing Laboratory for IVD Medical Devi
 China OECD GLP-Certified Laboratory
China OECD GLP-Certified Laboratory
Leave us a message
24-hour online customer service at any time to respond, so that you worry!




