
FDA ASCA Accreditation for Chinese Laboratory
FDA ASCA Program Overview
The Accreditation Scheme for Conformity Assessment (ASCA) is an initiative implemented by the FDA based on amendments to Section 514 of the Federal Food, Drug, and Cosmetic Act in 2017 and the Medical Device User Fee Amendments of 2017. This program aims to reduce regulatory burdens by increasing the FDA’s confidence in medical device testing methods and results, ensuring that patients receive safe, effective, and high-quality medical devices.
Before participating in the FDA ASCA program, biocompatibility laboratories must first obtain ISO 17025 accreditation and comply with FDA Good Laboratory Practice (GLP) requirements. Only then can they submit an ASCA accreditation application to the FDA.
ASCA Recognized Standards and Testing Methods
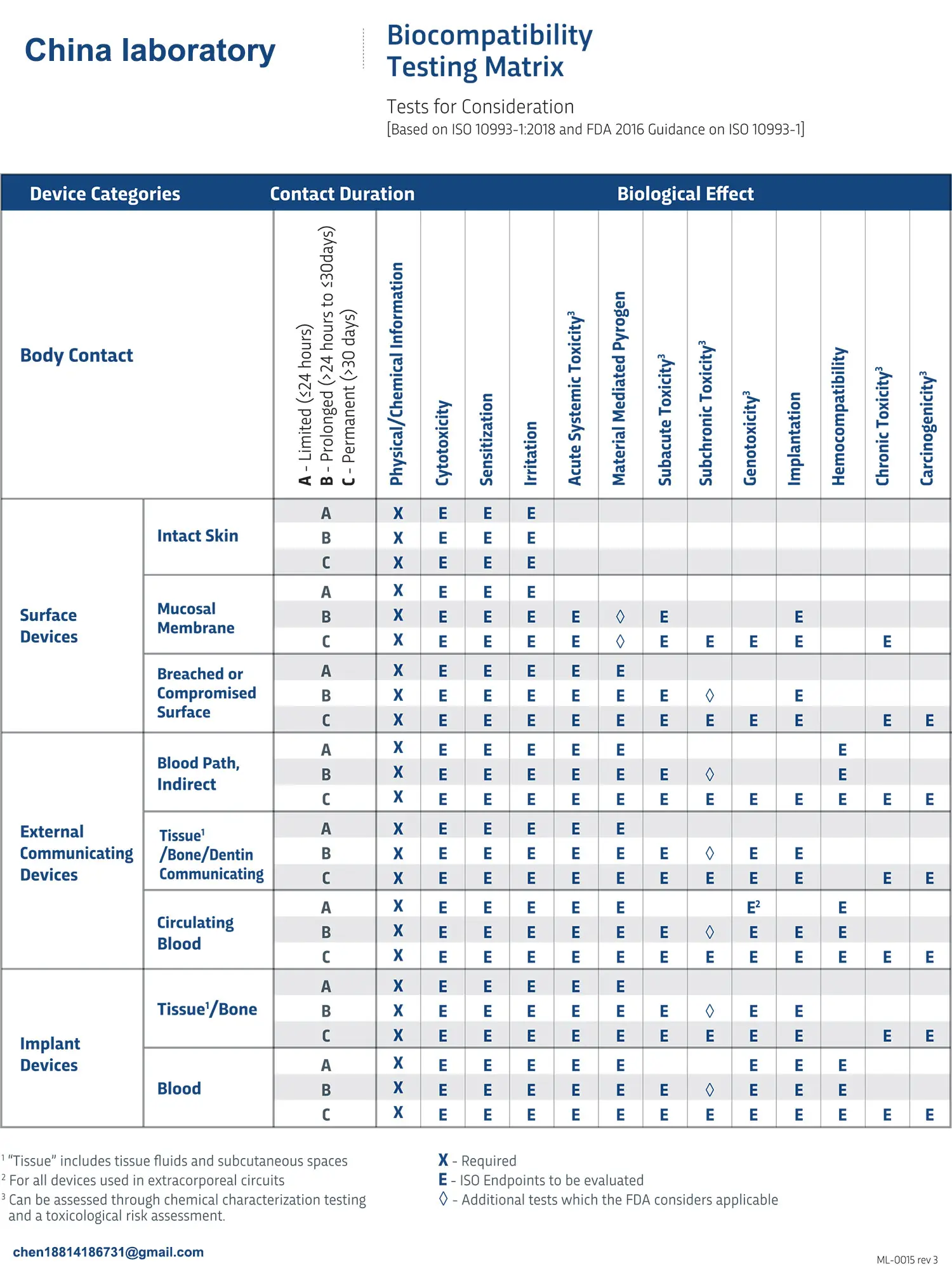
FDA-Recognized Consensus Standards for Biocompatibility Testing of Medical Devices
- ISO 10993-4: Complement activation test – U.S. FDA-listed commercial ELISA kits
- ISO 10993-4 and ASTM F756: Direct and indirect hemolysis tests
- ISO 10993-5: MEM elution cytotoxicity test
- iso 10993-10: Skin sensitization; intracutaneous reactivity; closed patch sensitization test
- ISO 10993-10 and ASTM F720: Guinea pig maximization sensitization test
- ISO 10993-11: Acute systemic toxicity test
- ISO 10993-11 and USP 151: Material-mediated pyrogen test
- ISO 10993-12: Sample preparation (all tests)
JJR Laboratory Medical Device Testing Center – ASCA Accreditation Scope
Since obtaining ASCA accreditation for hemolysis and MEM elution cytotoxicity testing in 2023, China's JJR Laboratory Medical Device Testing Center has become the only ASCA-accredited biocompatibility laboratory in the Asia-Pacific region (as of the publication date).
In July 2024, JJR Laboratory submitted an application for an expanded ASCA accreditation for complement activation testing, which was approved by the FDA after four months. This means that JJR Laboratory is now fully equipped to conduct all in vitro ASCA biocompatibility tests.
As of the publication date, JJR Laboratory ranks second globally in ASCA biocompatibility testing capabilities.
Medical Devices Requiring Complement Activation Testing
Medical devices that directly contact circulating blood are categorized into externally communicating devices and implantable devices. According to FDA recommendations, hemolysis, complement activation, and thrombogenicity testing should be considered for all such devices, regardless of the contact duration.
Common externally communicating devices requiring complement activation testing include:
- Extracorporeal membrane oxygenators
- Hemodialyzers / Hemofilters
- Cardiovascular interventional devices
- Intravascular catheters (balloon, imaging, laser, ultrasound)
- Intravascular guidewires
- Coronary retrograde perfusion catheters
Common implantable devices requiring complement activation testing include:
- Circulatory assist devices (ventricular assist devices, artificial hearts, intra-aortic balloon pumps)
- Intravenous synthetic vascular grafts
- Drug-eluting intravascular catheters
- Intravascular oxygenators (artificial lungs)
- Mechanical or biological heart valves
- Surgical synthetic or biological vascular grafts
Complement Activation Testing Procedures
SC5b-9 is considered the most critical marker representing the overall degree of complement activation. By quantitatively measuring terminal complement complex SC5b-9, it is possible to assess whether a test article has potential complement activation properties.
Key Considerations for Complement Activation Testing:
1. Testing must be conducted on the final medical device product.
2. Comparison with FDA-approved or destination market-approved competitor products is recommended (must provide corresponding registration certificate numbers).
3. U.S. FDA-listed commercial assay kits must be used.
4. The test must include appropriate controls and reference materials.
5. Results should be evaluated using statistical methods.
Significance of ASCA Accreditation for Complement Activation Testing
The FDA ASCA accreditation for complement activation testing is granted based on rigorous assessments of:
- Laboratory personnel qualifications
- Testing methods and procedures
- Overall quality management systems
Advantages of Testing in an ASCA-Accredited Laboratory:
- High credibility of test results and data
- Compliance with FDA requirements for test reports
- Concise summary reports that significantly reduce FDA review time
- Faster regulatory submissions for medical device manufacturers
In February 2024, the FDA issued a public communication reminding medical device manufacturers to carefully evaluate third-party laboratories conducting performance testing. The FDA strongly encourages collaboration with ASCA-accredited laboratories to ensure the authenticity and accuracy of data submitted.
Recent FDA statistical reports suggest that choosing an FDA ASCA-accredited laboratory for testing can substantially improve the FDA’s confidence in test report data quality and completeness. This leads to shorter FDA review times and increased efficiency in medical device regulatory submissions.
Email:hello@jjrlab.com
Write your message here and send it to us
 Toothbrush FDA Certification Testing
Toothbrush FDA Certification Testing
 Snoring Device FDA 510k Standard Testing
Snoring Device FDA 510k Standard Testing
 Single Use Intravenous Catheter Certification Test
Single Use Intravenous Catheter Certification Test
 Silicone Material Product Compliance Certification
Silicone Material Product Compliance Certification
 What to Do If Cytotoxicity Test Results Are Positi
What to Do If Cytotoxicity Test Results Are Positi
 ISO 10993:5 Cytotoxicity Testing Methods
ISO 10993:5 Cytotoxicity Testing Methods
 FDA ISO 10993-1 Biocompatibility Evaluation Guidel
FDA ISO 10993-1 Biocompatibility Evaluation Guidel
 In Vitro Cytotoxicity Testing for Medical Devices
In Vitro Cytotoxicity Testing for Medical Devices
Leave us a message
24-hour online customer service at any time to respond, so that you worry!




