
Brief Introduction to Biocompatibility
The Role of biocompatibility testing in Modern Medicine
In the field of modern healthcare, medical devices act like magical keys that unlock humanity's ability to combat diseases and safeguard health. These devices are diverse, with varied functions: some, like pacemakers, revive failing hearts; others, like artificial joints, restore mobility; still others, like medical catheters, silently deliver medications and fluids. However, for these devices to function safely within the human body, they must pass a critical checkpoint—biocompatibility testing.
Importance of Biocompatibility Testing
Biocompatibility testing is akin to a strict "gatekeeper," meticULously examining every device attempting to enter the human body. If the human body is a complex ecosystem, medical devices are "foreign guests" intruding on this system. The goal of biocompatibility testing is to ensure these "guests" can coexist harmoniously with their "host"—the human body—without causing adverse reactions like localized inflammation, immune rejection, or blood clot formation, thereby safeguarding health and safety.
Key Aspects of Testing
- cytotoxicity testing: Cells are the basic units of the human body, akin to the bricks building a skyscraper. Cytotoxicity testing evaluates the "interaction" between device materials and cells. If the material releases toxic substances, like poison into calm waters, it can alter cell morphology, cause vacuolization, detachment, or even cell lysis, undermining the body’s foundation.
- sensitization testing: The immune system is like a vigilant guard, constantly monitoring for foreign invaders. Sensitization testing identifies whether a device triggers an immune overreaction. Certain materials might be recognized as antigens, causing allergic reactions like rashes, itching, or difficulty breathing—akin to a sudden storm disrupting a peaceful day.
- Hemocompatibility Testing: Blood circulates continuously, transporting nutrients, oxygen, and waste, like a river within the body. Hemocompatibility testing evaluates whether a device interferes with blood flow or function, such as inducing platelet aggregation and thrombosis (blocking the "river") or hemolysis (rupturing RED blood cells), disrupting the "river’s" role in transporting oxygen.
- Implant Testing: For long-term implants like artificial joints or heart stents, implant testing is vital. By implanting devices into animal models, researchers observe local reactions and tissue compatibility over time—akin to testing weapons on a simulated battlefield. This ensures the device integrates well without causing inflammation, necrosis, or fibrosis.
Standards and Regulations
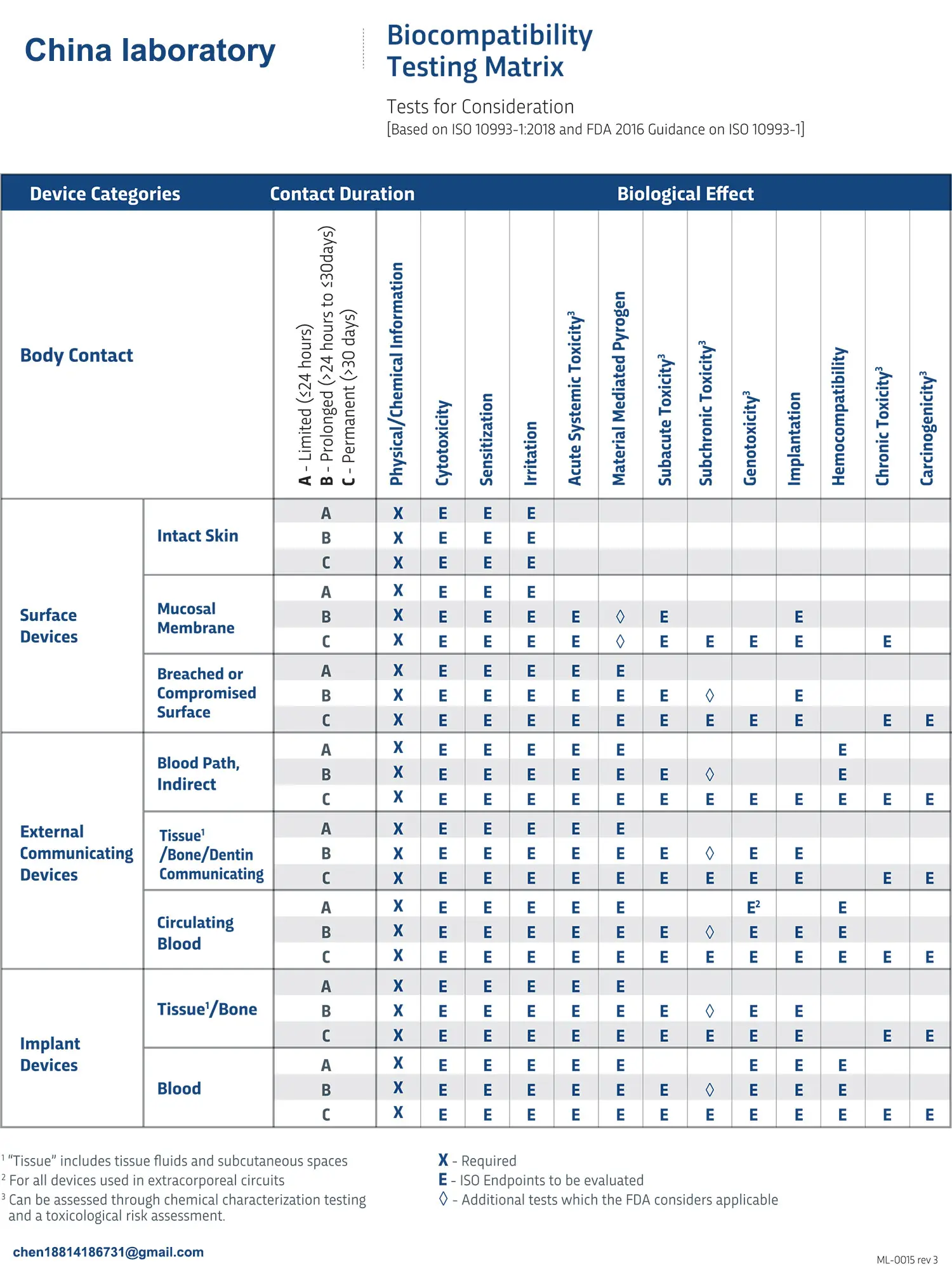
Biocompatibility testing adheres to strict standards and regulations, much like traffic rules ensure orderly roads. The ISO 10993 series, established by the International Organization for Standardization (ISO), serves as the "traffic law" in this domain, detailing requirements for test methods, sample preparation, animal selection, and result evaluation. Regulatory bodies worldwide adapt these standards to their national contexts to ensure stringent pre-market testing.
Selecting Testing Organizations
In the "world of testing," numerous professional institutions operate like schools of martial arts, each with unique "skills" and strengths. Comprehensive organizations offer one-stop testing services, while specialized institutions excel in biocompatibility testing. Choosing the right testing organization requires evaluating qualifications, reputation, and service quality to ensure accurate and reliable results.
Frequently Asked Questions (FAQs)
1. Do all medical devices require biocompatibility testing?
- Not all devices need full biocompatibility testing. High-risk devices with prolonged body contact, like implants, require extensive testing, while low-risk devices may need only partial testing.
2. How long does biocompatibility testing take?
- Testing duration varies. Simple tests like cytotoxicity may take days to weeks, while complex implant tests can span months to years.
3. What are the costs of biocompatibility testing?
- Costs range from $600–$3,000 per test, with full testing suites costing thousands to tens of thousands of dollars.
4. What happens if a device fails testing?
- Manufacturers must improve materials or designs until standards are met; otherwise, market approval will be denied.
5. Can biocompatibility testing replace clinical trials?
- No. Laboratory testing evaluates compatibility, while clinical trials assess overall safety and efficacy in real-world conditions.
6. How is testing accuracy ensured?
- Institutions must adhere to standards, maintain stable environments, and implement strict quality controls, from sample preparation to data analysis.
7. What are the trends in biocompatibility testing?
- Advances include more sensitive, accurate methods that better simulate human physiology, alongside personalized approaches for tailored medical device selection.
8. How do domestic and international standards differ?
- While broadly similar, differences arise in animal selection, test methods, and result interpretation due to regulatory and cultural factors.
9. What impact does biocompatibility testing have on the industry?
- It ensures quality and safety, drives innovation, and promotes industry standardization and professionalism.
10. Can patients access testing results?
- Yes, patients have the right to know testing outcomes. Manufacturers and healthcare providers should provide necessary information to aid informed decisions.
Email:hello@jjrlab.com
Write your message here and send it to us
 Cost of U.S. FDA CFR 21 177.2600 Test Report
Cost of U.S. FDA CFR 21 177.2600 Test Report
 How much does the IP44 Compliance Test cost
How much does the IP44 Compliance Test cost
 What is LFGB Test
What is LFGB Test
 What does LFGB certified mean?
What does LFGB certified mean?
 Weee authorised representative germany
Weee authorised representative germany
 Where to Apply for 2026 Air & Sea Transport Ce
Where to Apply for 2026 Air & Sea Transport Ce
 Guide to IEC Test Reports for Lighting Exports
Guide to IEC Test Reports for Lighting Exports
 IEC/EN 62471 and IEC/EN 62778 (Photobiological Saf
IEC/EN 62471 and IEC/EN 62778 (Photobiological Saf
Leave us a message
24-hour online customer service at any time to respond, so that you worry!




