
Biocompatibility Evaluation of Medical Devices
Biocompatibility is an important indicator for ensuring the safety of medical devices, and its research and analysis must be carried out throughout the project, occupying significant financial, human, and time resources. Many professionals in the industry are apprehensive about "biocompatibility," but once the principles are understood, the evaluation process becomes quite simple. During the early stages of product development and project initiation, the costs associated with biocompatibility can often be transferred to upstream suppliers, who are required to provide relevant proof documents and sign quality agreements that outline the supplier's responsibilities and risks.
However, for the final product (the product that can be marketed), the company itself must conduct the evaluation and analysis. In most cases, many companies passively and reluctantly choose to conduct biocompatibility testing (final evaluation testing), opting to conduct more tests rather than fewer. This inevitably leads to a waste of resources and costs, resulting in "over-research." This article discusses the overall approach to evaluating the biocompatibility of final products based on the actual situation of enterprises.
Biocompatibility Evaluation Can Be Divided into Three Main Scenarios:
1. No Biocompatibility Evaluation Required
Medical devices that do not come into direct or indirect contact with the human body and do not trigger biological stress responses in the tissue, such as in vitro diagnostic reagents (IVD), biochemical analyzers, and MRI devices, do not require biocompatibility evaluation. In this case, a simple statement explaining the product's intended use is sufficient to complete the evaluation.
2. Comparison with Similar Products
This method, also known as the "overall evaluation approach," involves demonstrating the biocompatibility and safety of the product based on a comparison with similar products. This approach is both loved and dreaded. The advantage is that no money needs to be spent to resolve the issue, which makes it highly favored by executives. The disadvantage is that if supporting documentation cannot be found, or if it is found but does not withstand scrutiny from evaluators, it becomes a significant challenge. The success of this approach depends on the experience and knowledge of the R&D staff, as it can be difficult to standardize the evaluation. The overall approach involves not selecting evaluation endpoints, meaning no biocompatibility tests are required, as long as sufficient evidence supports the safety of the biological hazards.
1. Data Collection
In simple terms, data from similar products is required, including but not limited to the following:
- Raw material information: including all material names and grades.
- Processing methods: including process flow diagrams, packaging methods, and sterilization methods of the comparison product.
- Model cross-comparisons: comparing the geometric and physical properties of the products.
- Clinical usage: the same clinical application method.
- Contact with the human body: choosing a downgraded approach, i.e., requiring shorter contact times for the declared product compared to the comparison product (e.g., the comparison product has a 7-day contact time, but the declared product has only a 2-day contact time, which is considered valid).
These data are typically confidential and are generally only accessible within the company or between subsidiaries and related companies.
2. Data Analysis and Conclusion
If the analysis shows no differences, the product passes the evaluation. If differences exist, further analysis or biocompatibility testing may be required for the differing aspects.
3. Final Evaluation Approach
If biocompatibility cannot be evaluated using the method in Section 2, then biocompatibility testing through the final evaluation approach must be employed. This is the most commonly used evaluation method today. The general approach is as follows:
1. Analyze the Characteristics of the Medical Device
- Contact with the Human Body:
- Surface contact: skin contact, mucosal contact, contact with broken or damaged surfaces.
- External connection: contact with indirect blood flow, contact with tissue/bone/dentin, contact with circulating blood.
- Implantable devices: contact with tissue/bone, contact with circulating blood.
- Contact Time Classification:
- Short-term contact: cumulative time < 24 hours.
- Long-term contact: cumulative time between 1 and 30 days.
- Permanent contact: cumulative time ≥ 30 days.
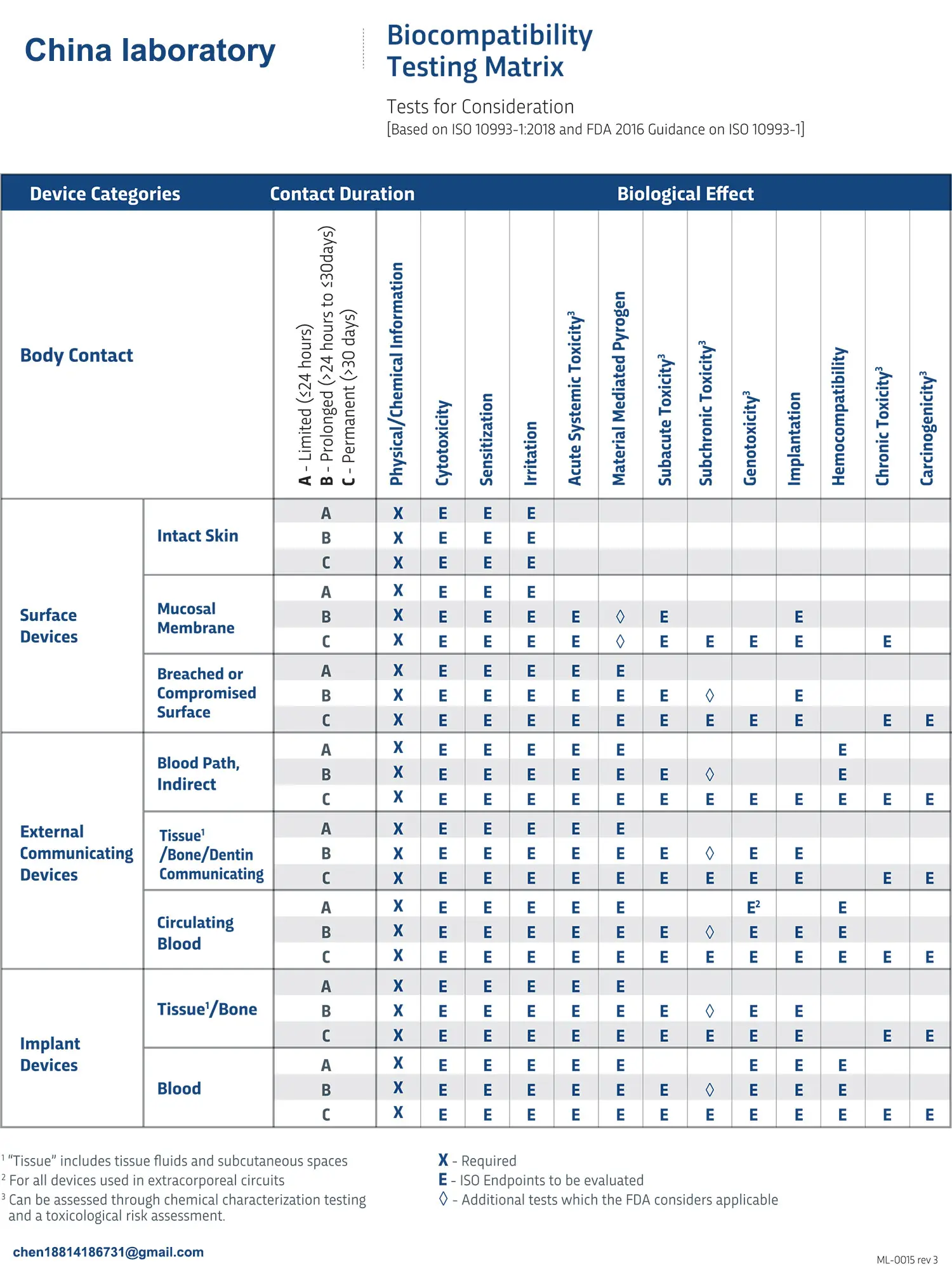
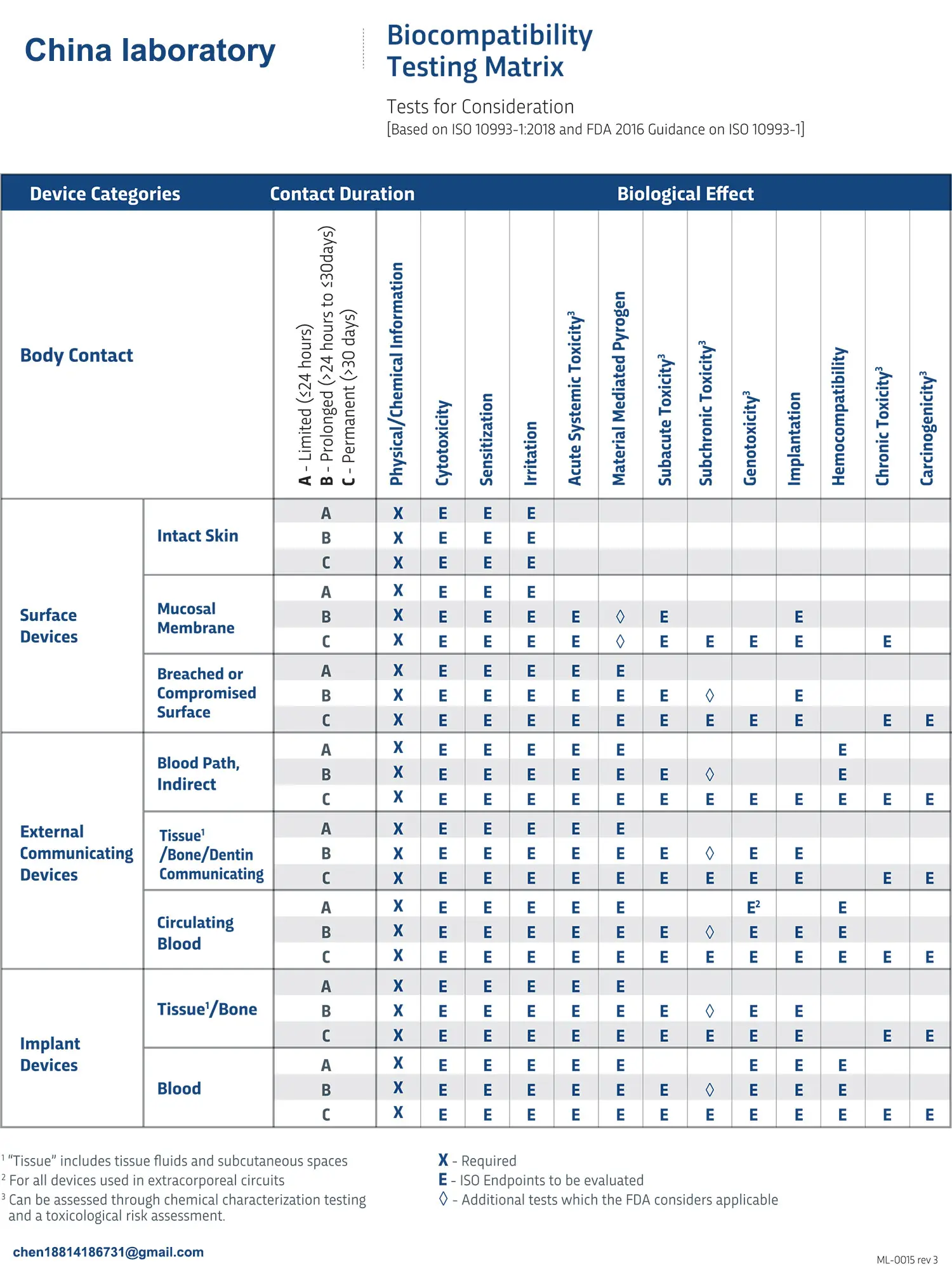
2. Select Endpoint Tests
Based on the above analysis, evaluate the declared product and select biological endpoint tests according to ISO 10993 Appendix A. For example, for a blood dialysis tube, the product should be classified as "contact with circulating blood and long-term contact." The biological evaluation endpoints may include: cytotoxicity, sensitization, irritation or intracutaneous reactions, material-mediated pyrogenicity, acute systemic toxicity, subacute toxicity, subchronic toxicity, chronic toxicity, implantation response, hemocompatibility, genotoxicity, and carcinogenicity.
3. Testing
Choose a qualified third-party testing agency to conduct the tests and provide a testing report.
4. Write the Biocompatibility Research Report
Based on the results of the biocompatibility tests, a conclusion should be drawn, and a biocompatibility research report should be compiled.
Email:hello@jjrlab.com
Write your message here and send it to us
 Toothbrush FDA Certification Testing
Toothbrush FDA Certification Testing
 Snoring Device FDA 510k Standard Testing
Snoring Device FDA 510k Standard Testing
 Single Use Intravenous Catheter Certification Test
Single Use Intravenous Catheter Certification Test
 Silicone Material Product Compliance Certification
Silicone Material Product Compliance Certification
 What to Do If Cytotoxicity Test Results Are Positi
What to Do If Cytotoxicity Test Results Are Positi
 ISO 10993:5 Cytotoxicity Testing Methods
ISO 10993:5 Cytotoxicity Testing Methods
 FDA ISO 10993-1 Biocompatibility Evaluation Guidel
FDA ISO 10993-1 Biocompatibility Evaluation Guidel
 In Vitro Cytotoxicity Testing for Medical Devices
In Vitro Cytotoxicity Testing for Medical Devices
Leave us a message
24-hour online customer service at any time to respond, so that you worry!




